FREE! Stop That Clot: Haemostasis and anticoagulants
2 hours
2 hours
ABSTRACT
This continuing professional development activity reviews the process of
haemostasis and the role of anticoagulant therapy in preventing
complications from abnormal clotting. Nurses are encountering increasing
numbers of clients in hospital and the community who are on prophylactic
or long-term anticoagulant therapy. Appreciation of the mechanisms of
coagulation and the rationale for advice given to clients prescribed
anticoagulant medication is essential to delivering effective care.
After completing this learning activity you should be able to:
- Outline the process of haemostasis and its controls.
- Discuss the causes and clinical outcomes of thrombus formation.
- Describe the actions of drugs in preventing or reversing thrombus formation.
- Provide rationales for common adverse events and advice given to clients while on anticoagulant drugs.
- Identify relevant laboratory tests used to assess haemostatic function and discuss the significance of test results.
The PDF accompanying this activity was first published in Kai Tiaki Nursing New Zealand in February 2011. It is not identical to the web activity.
Introduction
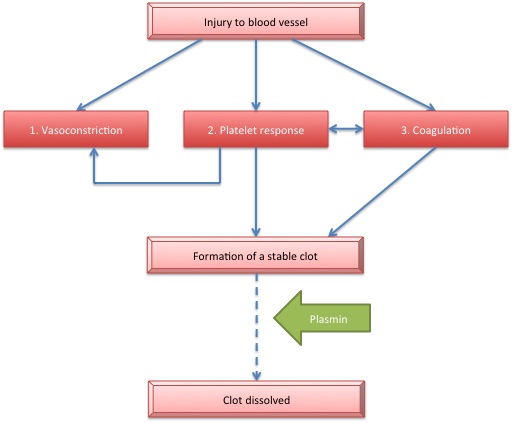
Haemostasis, the formation of a stable blood clot, occurs in three phases. Vasoconstriction occurs immediately following injury to a blood vessel. This slows blood flow in the area enhancing platelet activation. Platelet activation and the triggering of the coagulation pathway form a stable fibrin clot that prevents further blood loss. The clot is dissolved by fibrinolysis as the blood vessel is repaired.The processes of haemostasis and clot lysis are controlled by a complex interaction of factors, co-factors and inhibitory proteins. The balance can be disrupted when pro-coagulant stimuli overwhelm anticoagulant or fibrinolytic mechanisms. In these circumstances, pharmacological intervention may be necessary.
Venous and arterial thrombi, with their associated risk of embolism, arise from numerous causes. The aging population, improved survival rates following major trauma or cardiac events, and improved methods for detection and diagnosis, mean that more people are now identified as having, or being at risk of developing, thromboemboli. Development of new, and more carefully targeted anticoagulant drugs has helped to reduce risks of prophylaxis. It is important for nurses to understand the role these drugs play in prevention of thrombus formation so we can provide best care for clients/patients both in acute and long term therapy.
Haemostasis
Haemostasis (Figure 1) is triggered where the endothelium (inner layer) of a blood vessel is damaged and blood components contact underlying tissues. Initially, damage to a blood vessel will stimulate contraction of smooth muscle in the blood vessel wall. Reduced velocity of flow decreases blood loss and allows platelet activation. Platelet factors, in turn, enhance smooth muscle constriction of the vessel.Figure One. Stages of Haemostasis